Diseases
Standard Treatment for Noncompliant Elderly Increases Death 60-70%
 The elderly who are diagnosed with Alzheimer’s disease and are not compliant, especially those in nursing homes, are now routinely given antipsychotic drugs. One in three nursing home patients diagnosed with dementia are drugged. Their rate of death is increased by 60-70%.
The elderly who are diagnosed with Alzheimer’s disease and are not compliant, especially those in nursing homes, are now routinely given antipsychotic drugs. One in three nursing home patients diagnosed with dementia are drugged. Their rate of death is increased by 60-70%.
Who says antipsychotics increase the death rate so much? The FDA! In a 2005 warning, “Public Health Advisory: Deaths with Antipsychotics in Elderly Patients with Behavioral Disturbances” and in 2008 with the equivalent warning regarding older “typical” antipsychotics, the FDA warned that antipsychotics increase the rate of death by 60-70%. As many as one in three nursing home residents are given these drugs.
What does modern medical science focus on? Do they search to find why elderly people become difficult in nursing homes? Do they try to figure out other methods to resolve the problem? (That is, of course, assuming it really is a problem, and not simply caretakers wanting an easy ride.) No, of course not! Medical pseudo science only tries to find out which drugs aren’t as bad.
The British Medical Journal (BMJ) has just published a study, “Differential risk of death in older residents in nursing homes prescribed specific antipsychotic drugs: population based cohort study” that focuses on how atypical antipsychotics compare with each other in elderly death rates. Fortunately, the authors were concerned with the fact that these drugs are dangerous and expressed it:
… most patients will be given a psychotropic drug at some point in their disease progression. In the absence of proved effective and safe alternative pharmacological treatments, it is likely that antipsychotic drugs will continue to be used widely, despite the fact that they have not been approved for this indication, their use cannot be justified as evidence based, and there are clear data confirming their associated risk.
The evidence provided in our study reinforces the important risks associated with the use of these drugs and underscores the need to try alternative means of dealing with behavioural problems in older patients with dementia. [Emphasis mine.]
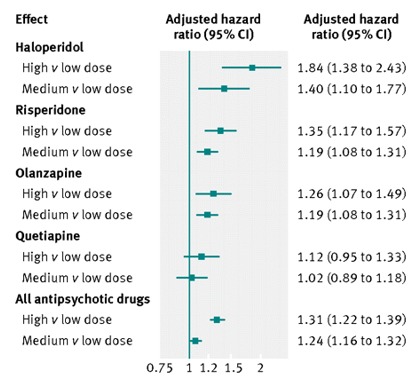 Nonetheless, their study was not about the dangers of antipsychotics; it was about which ones are worse than others. To the left is a graph they produced that gives their results. Notice that the comparisons are only between high or medium doses versus low doses.
Nonetheless, their study was not about the dangers of antipsychotics; it was about which ones are worse than others. To the left is a graph they produced that gives their results. Notice that the comparisons are only between high or medium doses versus low doses.
The atypical antipsychotic drugs examined were Haldol (haloperidol), Risperdal (risperdone), Zyprexa (olanzapine), and Seroquel (quetiapine), Abilify (aripiprazole), and Geodon (ziprasidone).
The study also compared survival probabilities, with risperidone as the baseline.
No comparisons with non-drugged patients were made.
The goal of the study was to find out which drug or drugs are the least harmful. Though the authors did state that attempts should be made to find alternatives, they stop short of denouncing the use of antipsychotics in the elderly, in spite of the fact that they have never been approved for that purpose.
Only Alzheimer’s Patients?
The consistently-used term for the elderly who are drugged with antipsychotics is “behavioral problem”. When it comes to these prescriptions, there doesn’t appear to be any requirement that patients be diagnosed with Alzheimer’s. It’s only when discussing the use of these drugs in the elderly that the diagnosis is brought up. However, there is never any diagnostic prerequisite for their prescription.
The fact is that these drugs are used on anyone of any age who is difficult. Autistic children are routinely given them. Children who disrupt classes in school are given them. People diagnosed with virtually anything are being given these drugs. Why should we believe that they’re given only to the elderly with Alzheimer’s?
For that matter, how can they be justified in any elderly person when the sole purpose is to drug them into submission? Though stated otherwise with clinical terms like “behavioral problems”, the simple fact is that these drugs are not being used for the benefit of the patients.
When did it become okay to use drugs solely for the benefit and convenience of the caretakers? Even if there were no adverse effects, how did this come to be the standard treatment of anyone?
Medscape reports that two researchers, Drs. McCleery and Fox, who wrote an editorial commentary about the research, stated:
Where care homes or community care services are inadequate and local clinical resources cannot compensate for them, doctors face genuine dilemmas about how to respond to distressed patients, relatives, and carers, often in ethically complex situations that involve a variety of risks. It is probably fair to say that many doctors think that the evidence based guidelines are not adequate for the day to day reality of practice.
Apparently, the lack of evidence hasn’t been much of a deterrent in the prescription of these drugs. If there were any genuine concern about the ethics, they wouldn’t prescribe them. But, it’s so much easier to drug noncompliant nursing home residents into submission.
By extrapolation from this study, it can be seen that some antipsychotics are killing the elderly at more than double the rate of the undrugged. It seems that the thinking of those who prescribe and administer them is: So what if the elderly die at more than double the rate? If they won’t go along with the program, then they’re too much trouble, anyway. If they die sooner, rather than later, then so much the better.
How else can describe it? For years, the drugs have come with a black box warning about the increased death rate. Research funding isn’t for finding out why patients become “difficult” or how to better deal with it. The clear message is: Compliance at any cost. If you won’t leave this world submissively by choice, then you’ll do so by force.
Tagged alzheimer’s ability, alzheimer’s antipsychotics, alzheimer’s disease, alzheimer’s haldol, alzheimer’s risperdal, alzheimer’s seroquel, alzheimer’s zyprexa, antipsychotics, antipsychotics kill, antipsychotics kill the elderly, conventional medicine, drugging nursing home patients, elderly behavioral problems, fda, noncompliant elderly patients, nursing homes, psychiatry, science